Volume 25, Issue 3 (August & September 2022)
J Arak Uni Med Sci 2022, 25(3): 436-449 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rostamkhani F, Ghamari M, Babakhani V, Merghati Khoei E S. Comparison of the Effectiveness of "Cognitive Behavioral Therapy" and "Acceptance and Commitment Therapy" on Sexual Function in Postmenopausal Women. J Arak Uni Med Sci 2022; 25 (3) :436-449
URL: http://jams.arakmu.ac.ir/article-1-7139-en.html
URL: http://jams.arakmu.ac.ir/article-1-7139-en.html
1- Department of Midwifery, Faculty of Nursing and Midwifery, Zanjan Branch, Islamic Azad University, Zanjan, Iran.
2- Department of Counseling, Faculty of Humanities, Abhar Branch, Islamic Azad University, Zanjan, Iran. ,ghamari.m@abhariau.ac.ir
3- Department of Counseling, Faculty of Humanities, Abhar Branch, Islamic Azad University, Zanjan, Iran.
4- Iranian National Center of Addiction Studies, Institution of Risk Behaviors Reduction, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Counseling, Faculty of Humanities, Abhar Branch, Islamic Azad University, Zanjan, Iran. ,
3- Department of Counseling, Faculty of Humanities, Abhar Branch, Islamic Azad University, Zanjan, Iran.
4- Iranian National Center of Addiction Studies, Institution of Risk Behaviors Reduction, Tehran University of Medical Sciences, Tehran, Iran.
Keywords: Cognitive Behavioral Therapy, Acceptance and Commitment Therapy, Sexual Function, Menopause
Full-Text [PDF 5615 kb]
(1740 Downloads)
| Abstract (HTML) (4384 Views)
Full-Text: (3330 Views)
Introduction
Menopause is a stage in a woman’s sexual life that is associated with physical, physiological, and psychological changes and often affects the sexual functions of middle-aged women [1, 2]. Sexual function is an important part of menopausal women’s life and changes in it, especially during menopause, can affect their health. The prevalence of sexual performance problems among all women is estimated between 25 and 63 %. This prevalence in post-menopausal women is even higher and ranges from 68 to 86.5% in different countries [7]. To improve sexual function, there are various psychological methods. Some of the basic approaches to work in the field of sexual knowledge and dysfunctional communication beliefs are cognitive and behavioral therapy (CBT) and acceptance and commitment therapy (ACT) [6, 13]. The aim of this study was to compare the effectiveness of CBT and ACT on the sexual function of postmenopausal women.
Materials and Methods
The current research method was quasi-experimental with a pre-test, post-test, and follow-up with a control group, which was implemented in health centers number 9, 14, and 17 in Zanjan city in 2019-2020. The statistical population of the study included postmenopausal women who had gone through menopause in the past five years and had an undesirable sexual function and were referred to the aforementioned health center in Zanjan from November to January 2019 to receive services. First, the “Female Sexual Function Index” was completed by 70 menopausal women in a targeted manner. Then, of women who scored less than 28 out of 36 in the above index, 45 people were eligible for selection and randomly assigned to three groups of 15 people (intervention 1, intervention 2, and control). The control group did not receive any intervention, while in the first group, the intervention of CBT and in the second group, the intervention of ACT were implemented, each in eight sessions. The “Female Sexual Function Index” questionnaire was used to measure the data. The data obtained from the research were analyzed through analysis of variance with repeated measurements and using SPSS software, version 24.
Results
The mean age of the CBT, ACT, and control groups was 52.20(3.12), 50.40(5.52), and 50.86(1.99) years. Using the ANOVA results, the mean age of the three groups did not differ significantly (P>0.05). Before analyzing the data, its assumptions were examined. The results of the Kolmogorov-Smirnov test for sexual function (P>0.05) indicated that the variables in question were normal. Also, the results of Levene’s and Box’s M tests were not significant (P>0.05). These findings suggest the equality of variances. Therefore, ANOVA with repeated measurements was used.
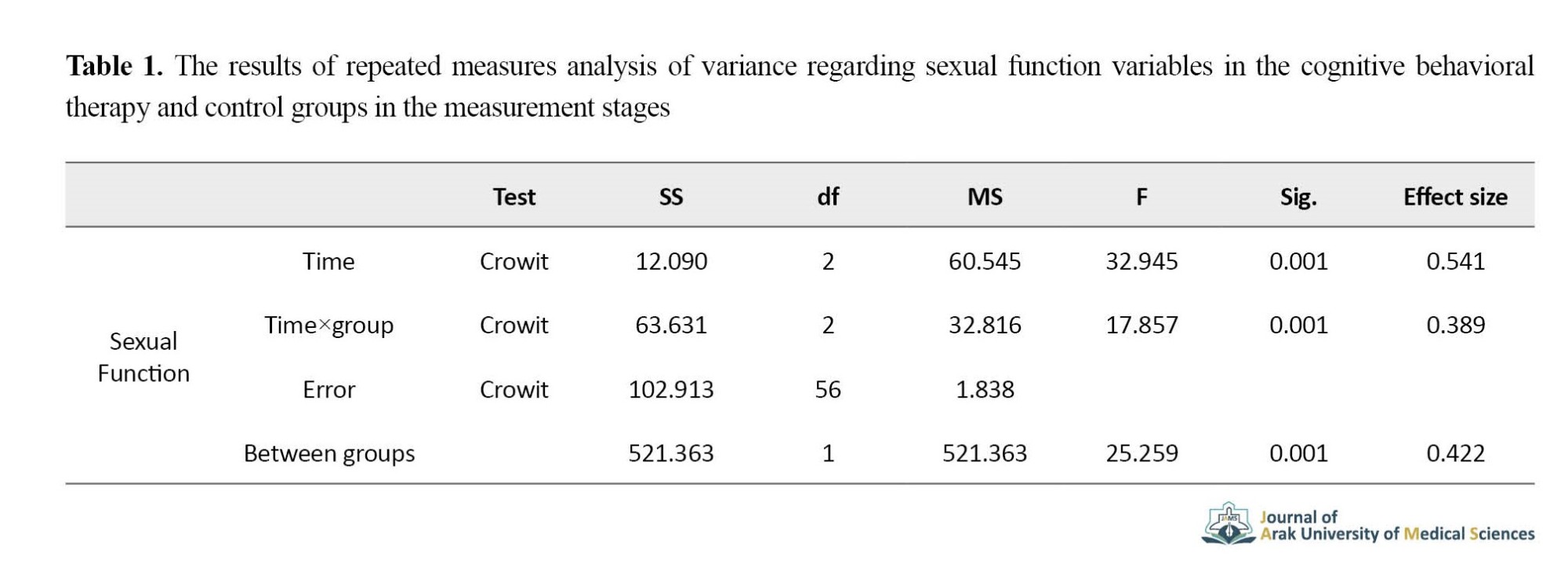
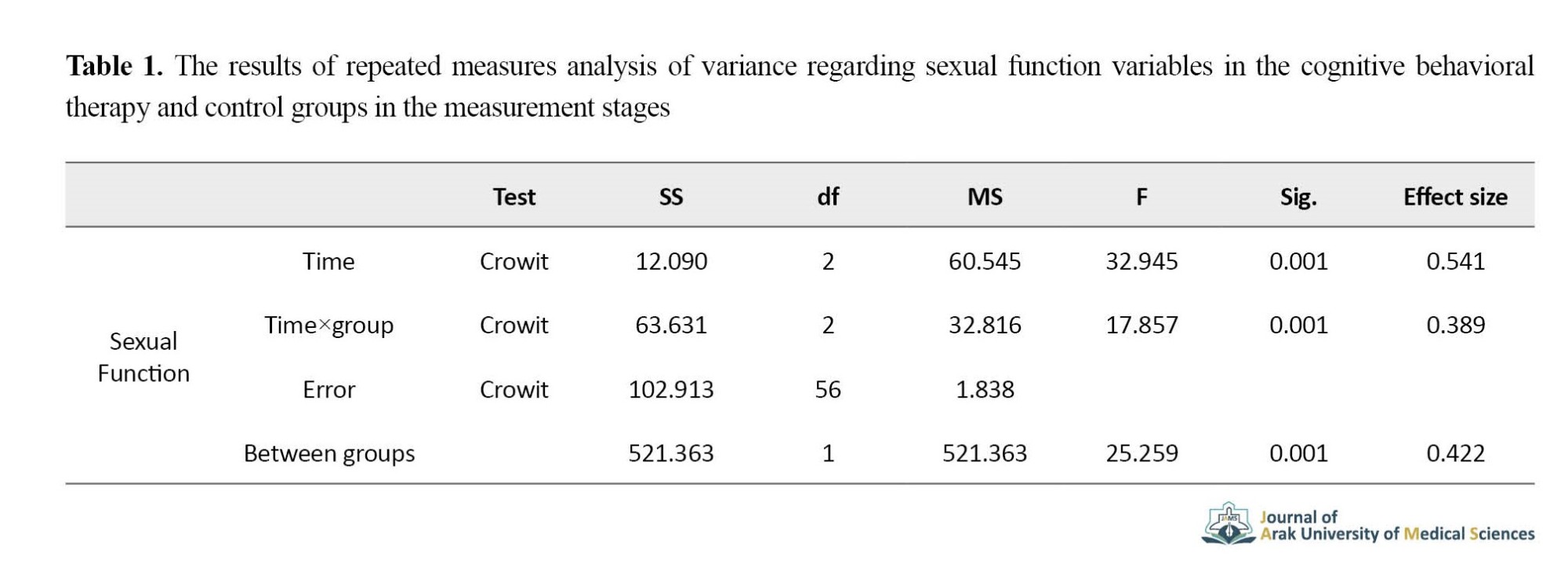
According to Table 1, the trend of changes in the CBT group compared to the control group in the measurement stages of sexual function variables (F=25.25 and P=0.001) was significantly different (P<0.05) and about 42% of observed differences in sexual function variables were due to group membership (intervention).
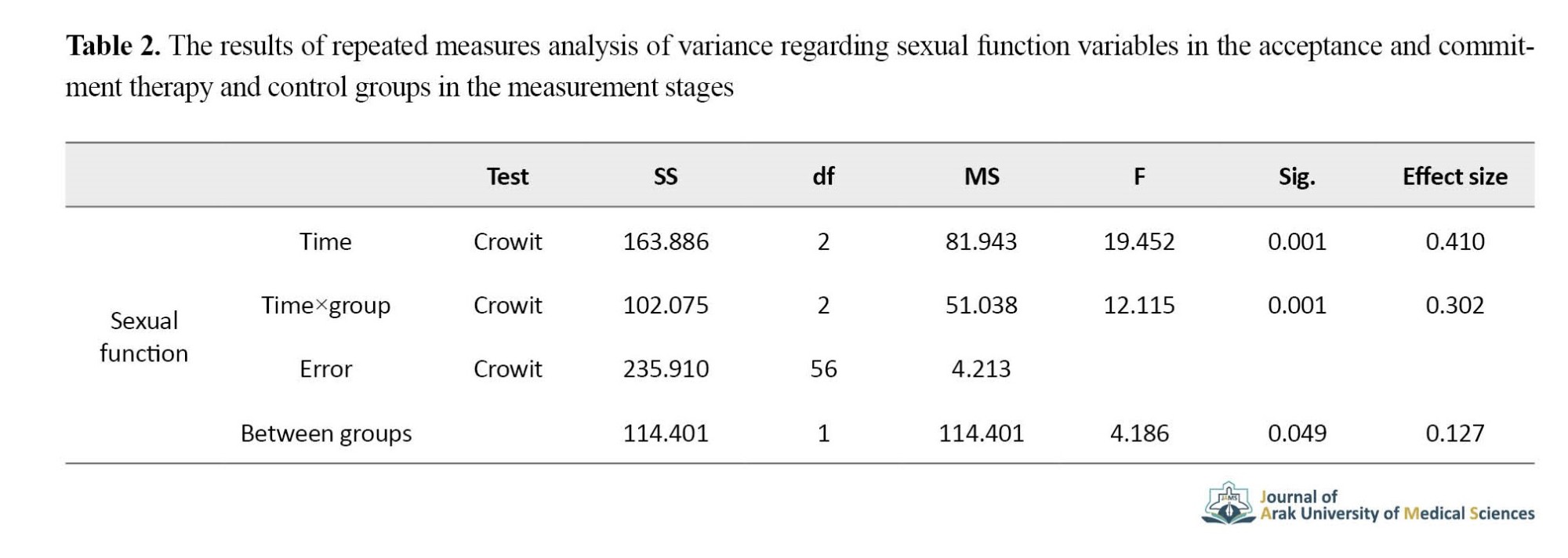
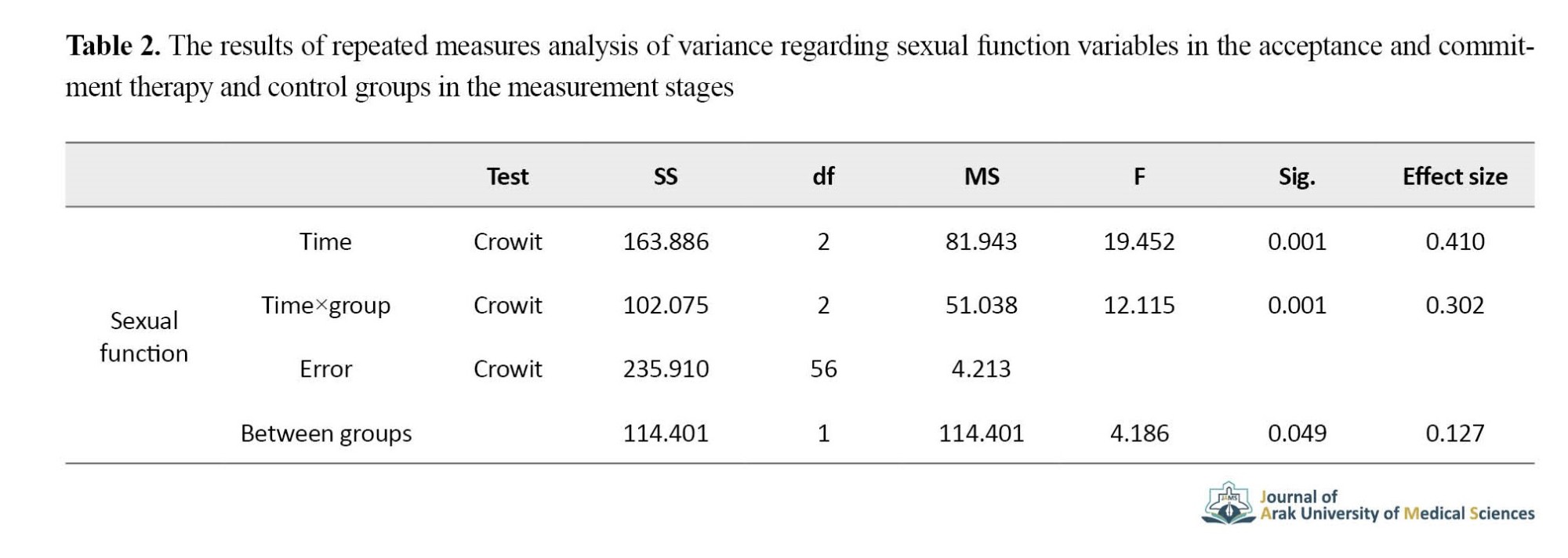
According to Table 2, the trend of changes in the ACT group compared to the control group in the stages of measurement in sexual function variables (F=4.186 and P=0.049) was significantly different (P<0.05) and 13% of observed differences in sexual performance variables were due to group membership (intervention). Regarding the intergroup effects, there was no statistically significant difference between the two intervention groups in sexual performance (F=0.004, P=0.952) (P<0.05).
Discussion
The purpose of this study was to compare the effectiveness of CBT and ACT on the sexual function of postmenopausal women. The results showed that after the intervention and follow-up, the level of sexual function among the intervention groups was significantly different from the control group, and the comparison of the averages also indicated an increasing trend after the implementation of the intervention. In other words, CBT and ACT improved the sexual function of postmenopausal women, and this effect was sustained for three months of follow-up. However, no significant difference was observed between the effectiveness of these two interventions on the sexual function of postmenopausal women. In explaining the results of the current research, it can be said that CBT with an increasing positive exchange, providing information in various fields, including sexual knowledge, changing dysfunctional misconceptions (cognitive distortions), cognitive reconstruction, creating problem-solving skills, and effective interpersonal relationships and negotiation increased the sexual function of postmenopausal women. CBT provides an opportunity for women to learn appropriate ways to identify and correct thoughts and methods of intercourse and sexual satisfaction and cognitive reconstruction to improve sexual disorders [34, 35, 4]. In explaining the effectiveness of ACT on sexual function, the results of many studies have shown that primarily many marital conflicts and dissatisfactions are caused by couples’ behavioral and psychological inflexibility with each other. On the other hand, ACT allows patients to change relationships with inner experiences, reduce experiential avoidance, increase psychological flexibility, and increase activity in a valuable path [41]. Considering that CBT and ACT treatments improved sexual function in postmenopausal women, it is suggested to use these treatments to improve the sexual function of postmenopausal women in health centers.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of the Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1398.328).
Funding
This article is the result of a PhD. student thesis by Rostamkhani Fatemeh in counseling and has not received any financial aid from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors sincerely appreciate the research vice-chancellor of Islamic Azad University, Abhar branch, the officials of the University of Medical Sciences and the colleagues of health centers in Zanjan city, and the women who participated in this research.
Menopause is a stage in a woman’s sexual life that is associated with physical, physiological, and psychological changes and often affects the sexual functions of middle-aged women [1, 2]. Sexual function is an important part of menopausal women’s life and changes in it, especially during menopause, can affect their health. The prevalence of sexual performance problems among all women is estimated between 25 and 63 %. This prevalence in post-menopausal women is even higher and ranges from 68 to 86.5% in different countries [7]. To improve sexual function, there are various psychological methods. Some of the basic approaches to work in the field of sexual knowledge and dysfunctional communication beliefs are cognitive and behavioral therapy (CBT) and acceptance and commitment therapy (ACT) [6, 13]. The aim of this study was to compare the effectiveness of CBT and ACT on the sexual function of postmenopausal women.
Materials and Methods
The current research method was quasi-experimental with a pre-test, post-test, and follow-up with a control group, which was implemented in health centers number 9, 14, and 17 in Zanjan city in 2019-2020. The statistical population of the study included postmenopausal women who had gone through menopause in the past five years and had an undesirable sexual function and were referred to the aforementioned health center in Zanjan from November to January 2019 to receive services. First, the “Female Sexual Function Index” was completed by 70 menopausal women in a targeted manner. Then, of women who scored less than 28 out of 36 in the above index, 45 people were eligible for selection and randomly assigned to three groups of 15 people (intervention 1, intervention 2, and control). The control group did not receive any intervention, while in the first group, the intervention of CBT and in the second group, the intervention of ACT were implemented, each in eight sessions. The “Female Sexual Function Index” questionnaire was used to measure the data. The data obtained from the research were analyzed through analysis of variance with repeated measurements and using SPSS software, version 24.
Results
The mean age of the CBT, ACT, and control groups was 52.20(3.12), 50.40(5.52), and 50.86(1.99) years. Using the ANOVA results, the mean age of the three groups did not differ significantly (P>0.05). Before analyzing the data, its assumptions were examined. The results of the Kolmogorov-Smirnov test for sexual function (P>0.05) indicated that the variables in question were normal. Also, the results of Levene’s and Box’s M tests were not significant (P>0.05). These findings suggest the equality of variances. Therefore, ANOVA with repeated measurements was used.
According to Table 1, the trend of changes in the CBT group compared to the control group in the measurement stages of sexual function variables (F=25.25 and P=0.001) was significantly different (P<0.05) and about 42% of observed differences in sexual function variables were due to group membership (intervention).
According to Table 2, the trend of changes in the ACT group compared to the control group in the stages of measurement in sexual function variables (F=4.186 and P=0.049) was significantly different (P<0.05) and 13% of observed differences in sexual performance variables were due to group membership (intervention). Regarding the intergroup effects, there was no statistically significant difference between the two intervention groups in sexual performance (F=0.004, P=0.952) (P<0.05).
Discussion
The purpose of this study was to compare the effectiveness of CBT and ACT on the sexual function of postmenopausal women. The results showed that after the intervention and follow-up, the level of sexual function among the intervention groups was significantly different from the control group, and the comparison of the averages also indicated an increasing trend after the implementation of the intervention. In other words, CBT and ACT improved the sexual function of postmenopausal women, and this effect was sustained for three months of follow-up. However, no significant difference was observed between the effectiveness of these two interventions on the sexual function of postmenopausal women. In explaining the results of the current research, it can be said that CBT with an increasing positive exchange, providing information in various fields, including sexual knowledge, changing dysfunctional misconceptions (cognitive distortions), cognitive reconstruction, creating problem-solving skills, and effective interpersonal relationships and negotiation increased the sexual function of postmenopausal women. CBT provides an opportunity for women to learn appropriate ways to identify and correct thoughts and methods of intercourse and sexual satisfaction and cognitive reconstruction to improve sexual disorders [34, 35, 4]. In explaining the effectiveness of ACT on sexual function, the results of many studies have shown that primarily many marital conflicts and dissatisfactions are caused by couples’ behavioral and psychological inflexibility with each other. On the other hand, ACT allows patients to change relationships with inner experiences, reduce experiential avoidance, increase psychological flexibility, and increase activity in a valuable path [41]. Considering that CBT and ACT treatments improved sexual function in postmenopausal women, it is suggested to use these treatments to improve the sexual function of postmenopausal women in health centers.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of the Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1398.328).
Funding
This article is the result of a PhD. student thesis by Rostamkhani Fatemeh in counseling and has not received any financial aid from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors sincerely appreciate the research vice-chancellor of Islamic Azad University, Abhar branch, the officials of the University of Medical Sciences and the colleagues of health centers in Zanjan city, and the women who participated in this research.
References
- Pourhosein R, Zarei J, Tarafdari A, Habibi Askar Abad M. [The relationship between gender schemas and the sexual health of postmenopausal women (Persian)]. J Psychol Dev. 2017; 6(3):191-212. [Link]
- Mojtabaei M, Saberi H, Alizadeh A. [The role of sexual schemas and body image on women’s sexual function (Persian)]. J Health Psychol. 2014; 3(1):52-64. [Link]
- Rajaeefard A, Beigi A, Salehi N. [Estimation of natural age of menopause in Iranian Women: A meta-analysis study (Persian)]. Koomesh. 2011: 13(1):1-7. [Link]
- Boland R, Verduin M, Ruiz P. Kaplan & Sadock’s synopsis of psychiatry. 12th ed. Philadelphia: Lippincott, Williams and Wilkinson; 2021. [Link]
- Nazarpour S, Simbar M, Ramezani Tehrani F. [Factors affecting sexual performance in menopause: A review of research texts (Persian)]. Payesh. 2014; 14(1):41-58. [Link]
- Goldenberg H, Goldenberg I. Family therapy: An overview. Nashvill: Broadman & Holman Publishers; 2011.
- Araoz D. Hypnosis in sexuality problems. Am J Clin Hypn. 2005; 47(4):229-42. [DOI:10.1080/00029157.2005.10403637] [PMID]
- Babakhani N, Taravati M, Masoumi Z, Garousian M, Faradmal J, Shayan A. The effect of cognitive-behavioral consultation on sexual function among women: A randomized clinical trial. J Caring Sci. 2018; 7(2):83-8. [DOI:10.15171/jcs.2018.013] [PMID] [PMCID]
- Haghighi H, Abedi P, Shirali Kh, Daraee R. [The effectiveness of Cognitive-Behavioral Therapy on reducing the sexual distress of postmenopausal women (Persian)]. Paper presented t: 14th Conference on Cognitive Behavioral Psychotherapy focusing on the transfer of clinical experiences among next-generation therapists. 15-17 May 2016; Tehran, Iran. [Link]
- Hummel SB, van Lankveld JJ, Oldenburg HS, Hahn DE, Broomans E, Aaronson NK. Internet-based cognitive behavioral therapy for sexual dysfunctions in women treated for breast cancer: Design of a multicenter, randomized controlled trial. BMC Cancer. 2015; 15:321. [DOI:10.1186/s12885-015-1320-z] [PMID] [PMCID]
- Shokhmgar Z, Rajaei A, Hossien Bayazi M, Teimory S. [The effect of group training on cognitive-behavioral therapy on marital satisfaction in infertile women applying for IVF (Persian)]. J Health Promot Manag. 2020; 9(4):1-11. [Link]
- Ramesh S, Rostami R, Marghati- Khoei E, Hemmat Boland E. [Effectiveness of combination of cognitive-behavioral therapy and biofeedback on vaginismus patients′ sexual function and marital status (Persian)]. Biannual J Appl Couns. 2016; 6(1):1-22. [DOI:10.22055/jac.2016.12565]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Publications; 1999. [Link]
- Izadi R, Abedi Mohammad R. [Acceptance and commitment-based therapy (Persian)]. Tehran: Jangal Publications; 2016. [Link]
- Eifert GH, Forsyth JP. Acceptance and commitment therapy for anxiety disorders: a practitioner’s treatment guide to using mindfulness, acceptance, and values-based behavior change strategies. Oakland CA: New Harbinger Publications; 2005. [Link]
- Luoma JB, Villatt JL. Mindfulness in the treatment of suicidal individuals. Cogn Behav Pract. 2012: 19(2): 265-76. [DOI:10.1016/j.cbpra.2010.12.003] [PMID] [PMCID]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, et al. A randomized controlled trial of mindfulness meditation versus relaxation training effects on distress. Positive states of mind rumination and distraction. Ann Behav Med. 2007: 33(1):11-21. [DOI:10.1207/s15324796abm3301_2] [PMID]
- Hasanzadeh M, Akbari B, Abolghasemi A. [Efficiency of acceptance and commitment therapy on psychological wellbeing and sexual function in women with infertility history (Persian)]. Avicenna J Nurs Midwifery care. 2020; 27(4):250-9. [DOI:10.30699/ajnmc.27.4.250]
- Tabatabayi AS, Sajjadian I, Motamedi M. [Effectiveness of acceptance and commitment therapy on sexual function, sexual self-consciousness and sexual assertiveness among women with sexual dysfunction (Persian)]. J Res Behav Sci. 2017; 15(1):84-92. [Link]
- Burpee LC, Langer EJ. Mindfulness and marital satisfaction. J Adult Dev. 2005; 12(1):43-51. [DOI:10.1007/s10804-005-1281-6]
- Azimifar S, Fatehizade M, Bahrami F, Ahmadi A, Abedi A. [Comparison of the effectiveness of cognitive-behavioral couple therapy and acceptance-based therapy and commitment to increase the marital happiness of dissatisfied couples (Persian)]. J Psychol Psychiatry. 2016: 3(2):56-81. [Link]
- kbari Torkestani N, Ramezannejad P, Abedi M, Eshrati B, Nekoobahr A, Ramezannejad P. [The effect of premarital counseling on the acceptance-based approach and commitment on sexual performance of couples (Persian)]. J Arak Uni Med Sci. 2016: 19(117):34-42. [Link]
- Khanjani Vashki S, Shafiabadi A, Farzad V, Fatehizadeh M. [A Comparison between the effectivness of cognitive-behavioral couple therapy and acceptance and commitment on marital intimacy of conflicting couples in Isfahan (Persian)]. J Knowl Res Appl Psychol. 2016: 17(4):31-40. [Link]
- Ghasemi S, Azizi A, Ismaili N. [Comparison of acceptance and commitment-based therapy with cognitive-behavioral therapy on marital satisfaction of women with obsessive-compulsive disorder in 2016 (Persian)]. J Community Health. 2017: 11(2):58-67. [DOI:10.22123/chj.2018.88102]
- Delavar A. [Applied probability and statistics in psychology and educational sciences (Persian)]. Tehran: Roshd Publication; 2014. [Link]
- Rosen R, Briwn C, Heimen J, Leiblum S, Maston R, Shabsigh D, et al. The Female Sexual Function Index (FSFI) a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26(2):191-208. [DOI:10.1080/009262300278597] [PMID]
- Mohammadi Kh, Heydari M, Faqihzadeh S. [The validity of the Persian version of the Female Sexual Function Index-FSFI scale as an indicator of women’s sexual performance (Persian)]. Monit Q. 2008; 7(2):269-78. [Link]
- Gibbs RS. Danforth’s obstetrics and gynecology. London: Lippincott Williams & Wilkins; 2008. [Link]
- Ter Kuile MM, Both S, Van Kankueld JJDM. Cognitive behavioral therapy for sexual dysfunction in woman. Psychiatr Clin North Am. 2010; 33(3):595-610. [DOI:10.1016/j.psc.2010.04.010] [PMID]
- Kaplan HS. The new sex therapy: Active treatment of sexual dysfunction. London: Psychology Press; 1974. [Link]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: The process and practice of mindful change. New York: Guilford Press; 2011. [Link]
- Rostamkhani F, Ghamari M, Babakhani V, Mergati Khoi A. [The effectiveness of cognitive-behavioral therapy on sexual function and sexual schemas in postmenopausal women (Persian)]. J Health Promot Manag. Tehran. 2020; 9(6):84-95. [Link]
- Brotto LA, Erskine Y, Carey M, Ehlen T, Finlayson S, Heywood M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012; 125(2):320-5. [DOI:10.1016/j.ygyno.2012.01.035] [PMID] [PMCID]
- Mutabi F, Fati L. [Therapeutic drawing in behavioral cognitive theory (Persian)]. 5th ed. Tehran: Danjeh Publications; 2016. [Link]
- Lavner JA, Karney BR, Bradbury TN. Does couples’ communication predict marital satisfaction, or does marital satisfaction predict communication? J Marriage Fam. 2016; 78(3):680-94. [DOI:10.1111/jomf.12301] [PMID] [PMCID]
- Rostamkhani F, Ghamari M, Babakhani V, Merghati KE. [The effect of acceptance and commitment therapy on sexual function in postmenopausal women (Persian)]. J Health Care. 2020; 22(2):102-13. [DOI:10.52547/jhc.22.2.102]
- Nazarpour S, Simbar M, Ramezani Tehrani F, Alavi Majd H. [Relationship between sexual function and quality of life in post-menopausal women (Persian)]. J Mazandaran Univ Med Sci. 2016; 26(143):88-98. [Link]
- Afghari A, Ganji J, Ahmadshirvani M. [Psycho-emotional changes in menopause: A qualitative study (Persian)]. J Mazandaran Univ Med Sci. 2012; 22(93):27-38. [Link]
- Hakimi S, Ramezani Tehrani F, Simbar M, Zaiery F. [Women’s experiences a bout menopause and related factors (Persian)]. Iran J Endocrinol Metab. 2017; 19(3):185-94. [Link]
- Iverach L, Menzies RG, O’Brian S, Packman A, Onslow M. Anxiety and stuttering: Continuing to explore a complex relationship. Am J Speech Lang Pathol. 2011; 20(3):221-32. [DOI:10.1044/1058-0360(2011/10-0091)] [PMID]
- Hayes SC, Strosahl KD. A practical guide to acceptance and commitment therapy. New York: Springer; 2010. [Link]
- Harris R, Hayes SC. ACT made simple: An easy- to- read primer on acceptance and commitment therapy. 2th ed. Oakland: New Harbinger Publications; 2019. [Link]
- Mojdeh F, Zeighami Mohamadi S. [The relationship between depression and sexual function index among married women (Persian)]. Avicenna J Nurs Midwifery Care. 2013: 21(1):41-51. [Link]
Type of Study: Original Atricle |
Subject:
Obstetrics & Gynocology
Received: 2022/02/26 | Accepted: 2022/12/17
Received: 2022/02/26 | Accepted: 2022/12/17
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








